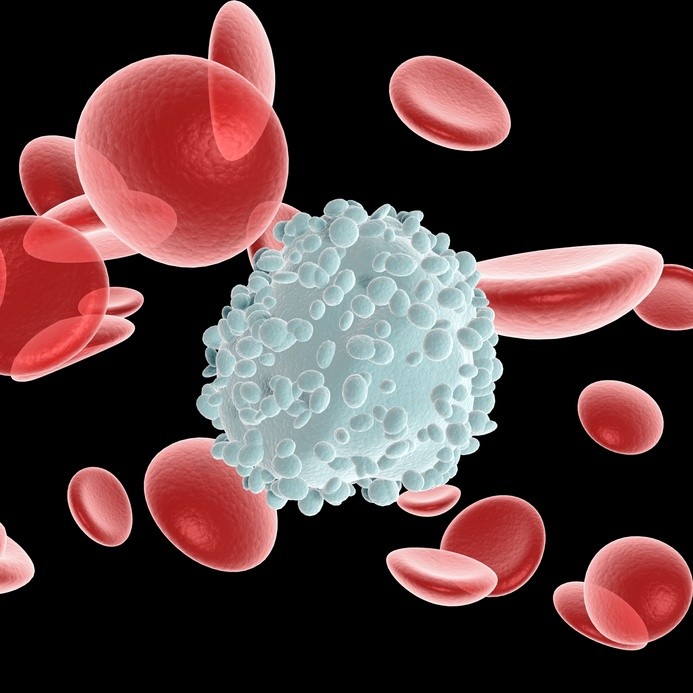
For the first time, scientists have turned human skin cells into transplantable white blood cells, soldiers of the immune system that fight infections and invaders. The work, done at the Salk Institute, could let researchers create therapies that introduce into the body new white blood cells capable of attacking diseased or cancerous cells or augmenting immune responses against other disorders.
The work, as detailed in the journal Stem Cells, shows that only a bit of creative manipulation is needed to turn skin cells into human white blood cells.
“The process is quick and safe in mice,” says senior author Juan Carlos Izpisua Belmonte, holder of Salk’s Roger Guillemin Chair. “It circumvents long-standing obstacles that have plagued the reprogramming of human cells for therapeutic and regenerative purposes.”
Those problems includes the long time — at least two months — and tedious laboratory work it takes to produce, characterize and differentiate induced pluripotent stem (iPS) cells, a method commonly used to grow new types of cells. Blood cells derived from iPS cells also have other obstacles: an inability to engraft into organs or bone marrow and a likelihood of developing tumors.
The new method takes just two weeks, does not produce tumors, and engrafts well.
“We tell skin cells to forget what they are and become what we tell them to be — in this case, white blood cells,” says one of the first authors and Salk researcher Ignacio Sancho-Martinez. “Only two biological molecules are needed to induce such cellular memory loss and to direct a new cell fate.”
Belmonte’s team developed the faster technique (called indirect lineage conversion) and previously demonstrated that these approaches could be used to produce human vascular cells, the ones that line blood vessels. Rather than reversing cells all the way back to a stem cell state before prompting them to turn into something else, such as in the case of iPS cells, the researchers “rewind” skin cells just enough to instruct them to form the more than 200 cell types that constitute the human body.
The technique demonstrated in this study uses a molecule called SOX2 to become somewhat plastic — the stage of losing their “memory” of being a specific cell type. Then, researchers use a genetic factor called miRNA125b that tells the cells that they are actually white blood cells.
The researchers are now conducting toxicology studies and cell transplantation proof-of-concept studies in advance of potential preclinical and clinical studies.
“It is fair to say that the promise of stem cell transplantation is now closer to realization,” Sancho-Martinez says.
Study co-authors include investigators from the Center of Regenerative Medicine in Barcelona, Spain, and the Centro de Investigacion Biomedica en Red de Enfermedades Raras in Madrid, Spain.
Story Source:
The above story is based on materials provided by Salk Institute for Biological Studies. Note: Materials may be edited for content and length.
Journal Reference:
- Julian Pulecio, Emmanuel Nivet, Ignacio Sancho-Martinez, Marianna Vitaloni, Guillermo Guenechea, Yun Xia, Leo Kurian, Ilir Dubova, Juan Bueren, Leopoldo Laricchia-Robbio, Juan Carlos Izpisua Belmonte. Conversion of Human Fibroblasts into Monocyte-Like Progenitor Cells. Stem Cells, 2014; DOI: 10.1002/stem.1800