Using human induced pluripotent stem cells (hiPSCs), researchers at Skaggs School of Pharmacy and Pharmaceutical Sciences at University of California, San Diego have discovered that neurons from patients with schizophrenia secrete higher amounts of three neurotransmitters broadly implicated in a range of psychiatric disorders.
The findings, reported online Sept. 11 in Stem Cell Reports, represent an important step toward understanding the chemical basis for schizophrenia, a chronic, severe and disabling brain disorder that affects an estimated one in 100 persons at some point in their lives. Currently, schizophrenia has no known definitive cause or cure and leaves no tell-tale physical marks in brain tissue.
“The study provides new insights into neurotransmitter mechanisms in schizophrenia that can lead to new drug targets and therapeutics,” said senior author Vivian Hook, PhD, a professor with Skaggs School of Pharmacy and UC San Diego School of Medicine.
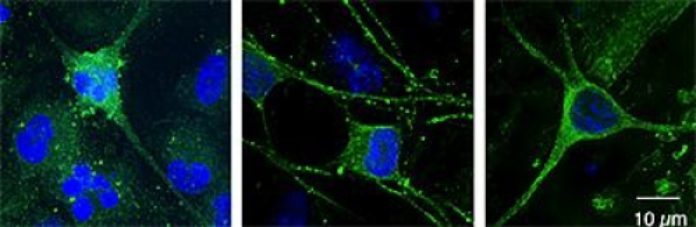
In the study, UC San Diego researchers with colleagues at The Salk Institute for Biological Studies and the Icahn School of Medicine at Mount Sinai, N.Y., created functioning neurons derived from hiPSCs, themselves reprogrammed from skin cells of schizophrenia patients. The approach allowed scientists to observe and stimulate human neurons in ways impossible in animal models or human subjects.
Researchers activated these neurons so that they would secrete neurotransmitters — chemicals that excite or inhibit the transmission of electrical signals through the brain. The process was replicated on stem cell lines from healthy adults.
A comparison of neurotransmitters produced by the cultured “brain in a dish” neurons showed that the neurons derived from schizophrenia patients secreted significantly greater amounts of the catecholamine neurotransmitters dopamine, norepinephrine and epinephrine.
Catecholamine neurotransmitters are synthesized from the amino acid tyrosine and the regulation of these neurotransmitters is known to be altered in a variety of psychiatric diseases. Several psychotropic drugs selectively target the activity of these neurotransmitters in the brain.
In addition to documenting aberrant neurotransmitter secretion from neurons derived from patients with schizophrenia, researchers also observed that more neurons were dedicated to the production of tyrosine hydroxylase, the first enzyme in the biosynthetic pathway for the synthesis of dopamine, from which both norepinephrine and epinephrine are made.
This discovery is significant because it offers a reason for why schizophrenia patients have altered catecholamine neurotransmitter levels: They are preprogrammed to have more of the neurons that make these neurotransmitters.
“All behavior has a neurochemical basis in the brain,” Hook said. “This study shows that it is possible to look at precise chemical changes in neurons of people with schizophrenia.”
The applications for future treatments include being able to evaluate the severity of an individual’s disease, identify different sub-types of the disease and pre-screen patients for drugs that would be most likely to help them. It also offers a way to test the efficacy of new drugs.
“It is very powerful to be able to see differences in neurons derived from individual patients and a big accomplishment in the field to develop a method that allows this,” Hook said.
Story Source:
The above story is based on materials provided by University of California, San Diego Health Sciences. Note: Materials may be edited for content and length.
Journal Reference:
- Vivian Hook, Kristen J. Brennand, Yongsung Kim, Thomas Toneff, Lydiane Funkelstein, Kelly C. Lee, Michael Ziegler, Fred H. Gage. Human iPSC Neurons Display Activity-Dependent Neurotransmitter Secretion: Aberrant Catecholamine Levels in Schizophrenia Neurons. Stem Cell Reports, 2014; DOI: 10.1016/j.stemcr.2014.08.001