As the Ebola epidemic in West Africa endures, some parallels are being drawn between the virus and HIV/AIDS. Both are spread by quite specific human behavior which is under conscious control: HIV by unprotected sex, Ebola by unsanitary burial practices, and both by contact with the bodily fluids of an infected person. However, with an incubation period of less than three weeks, Ebola progresses from infection to infectiousness more than 100 times as fast as untreated HIV. Thus, Ebola is like a pre-treatment HIV epidemic on steroids. So what can we learn from the global response to HIV/AIDS that can be applied to the Ebola response? There are a number of lessons (highlighted here and here), but I think the most relevant is that donors must give highest priority to helping affected African governments to protect health workers.
Before the arrival of HIV, medical personnel around the world had not feared infection from their patients since antibiotics had become widely available in the 1950s. Even in a country with a weak health system, virtually any infection a health worker acquired could be cured with the antibiotics to which health workers had priority access. For health workers in Africa, this sense of security evaporated in the 1980s, when AIDS was spreading and the virus called HIV had just been identified. Any patient arriving at a health center might be infected with HIV. Thus a health worker who accidentally stuck himself with a contaminated needle or inadvertently rubbed a patient’s blood or saliva onto his own open wound, might catch HIV. At that time there was no treatment for HIV infection, so each infection meant that, after an “incubation period” of 8 to 12 years, the health worker, like any HIV-infected person, would sicken and die of AIDS.
As the danger of HIV infection became widely understood, but before treatment was available, worried health workers were reluctant to go to work or to treat new patients. Patients whose blood tested positive for HIV were often placed in separate “AIDS wards” and subsequently neglected by fearful health workers. Entire hospitals would sometimes refuse to admit HIV positive patients, for fear that the public would designate the hospital an “AIDS hospital” and shun it.
Now we see health workers in the African countries of Guinea, Liberia, Sierra Leone, and Nigeria faced with similar, though more urgent challenges. Just as in the early days of HIV, African public health officials and their government and donor supporters must today be concerned with how to protect health workers from the Ebola infection so that the providers (a) stay free of infection; (b) feel secure enough to go to work; (c) prevent transmission from an infected patient to an uninfected one; (d) continue to provide good care to routine patients and (e) provide both care and comfort to the infected patient.
In the 1980s and ‘90s the policy tool that succeeded in accomplishing all these objectives for HIV was the definition and promulgation of so-called “universal precautions” for health workers. Since health workers had no quick way of knowing which new patient might be HIV positive, the World Health organization defined precautions that health workers should take “universally,” that is, for all patients. These included simple precautions like hand-washing before contact with each patient, face masks, gowns and rubber gloves. Helped by the spread of the information that HIV could not be transmitted by casual contact, donor and African government support for “universal precautions” alleviated health worker fears of HIV and of HIV-infected patients, kept workers on the job, and led to improved treatment of HIV-positive patients.
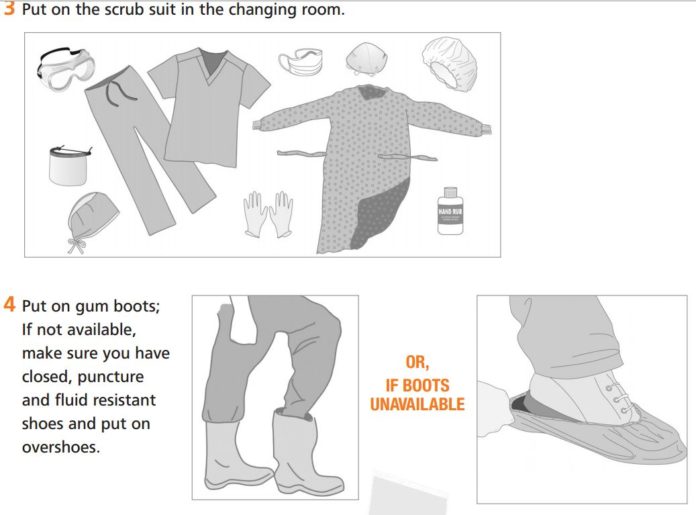
Similarly, the following figure, extracted from Annex 2 of the newly updated WHO guidelines, dramatically communicates how carefully health workers are advised to protect themselves from Ebola:

Figure: Steps 3-4 of ten “Steps to put on Personal Protective Equipment (PPE)” from Annex 2 of “Interim Infection Prevention and Control Guidance for Care of Patients with Suspected or Confirmed Filovirus Haemorrhagic Fever in Health-Care Settings, with Focus on Ebola,” World Health Organization, August 2014
Thanks to decades and billions of dollars of donor support for the battle against HIV, many African health facilities now have the rubber gloves, goggles, and face masks that were defined as the “universal precautions” to protect against HIV infection. But few yet have enough complete sets of gowns, masks, hair coverings, aprons, and rubber boots depicted in the guidelines to protect staff from Ebola. And fewer still have trained all their staff, including cleaners, orderlies, clerks and receptionists, in the proper techniques for putting on, removing and discarding or sterilizing this equipment. African health systems are better prepared for Ebola than they would have been without the HIV epidemic. But as the figure illustrates, much more protective gear is needed against Ebola than against HIV. And as my colleague Charles Kenny points out in a recent article, countries like Sierra Leone where health expenditure is only 26 cents per day do not have the resources to protect their own health workers from this new threat.
Donors must mobilize emergency task forces to procure and transport this full-body protective gear to all health facilities in the affected countries. And donors must help governments to distribute this gear and train their health providers in its use. Private providers, including pharmacists, must receive the same training as those in the public sector. Where African governments supplement their health personnel with village-based community health workers and traditional healers, they too must receive equipment and training. Since most caregivers are women, most of the gear must be distributed to women.
Just as universal precautions eased the concerns of health workers about on-the-job HIV infection in the 1980s and ‘90s, these new rigorous precautions can play a critical role in sustaining the existing health care systems as they control the Ebola epidemic. But given the rapid incubation period of Ebola, speedy donor action is even more important. Thanks to decades of lessons learned from the global HIV/AIDS response, we know more about how to respond to an epidemic like this. But donors and governments must act far more quickly to implement these lessons learned, support national health systems, and protect African health workers as a means to controlling this devastating new epidemic.