One of the greatest success stories in modern medicine is that HIV is no longer a death sentence, but a chronic, manageable disease that often can be managed with a single tablet a day.
Antiretroviral therapy (ART) is non-toxic, has very few side-effects and dramatically reduces a personʼs infectiousness. So weʼve seen dramatic reductions in HIV incidences globally; 50 countries last year reported a 25% decline in new HIV infections.
But there are still two and a half million infections occurring globally every year, and close to two million deaths. HIV is still with us and remains a significant problem.
Seeing an end of AIDS with therapy alone means finding, diagnosing and treating everyone with HIV, and once you start treatment, youʼre on it for the rest of your life. Thatʼs why there’s still interest in finding a cure for HIV, or a way for people to no longer need to take lifelong treatment.
Ability to rebound
When you start someone on ART, the virus very rapidly disappears from the blood. In fact, within a month, a person can have over a million copies of the virus per millilitre of blood fall to undetectable levels. At the same time, immune systems recover in most patients.
But as soon as you stop treatment – whether you’ve been on treatment for three years or 20 years, whether you started it shortly after infection or many years later – the virus comes straight back up, and in most people this is within two to three weeks. So although this virus is almost undetectable, itʼs always persistent and present.
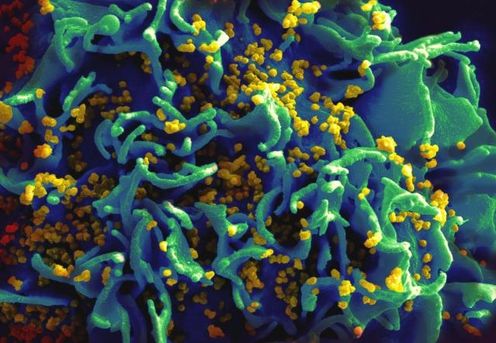
HIV is an RNA virus, which, when it gets to its target cell, copies itself backwards – what we call reverse transcription – and becomes DNA. And if you measure HIV DNA – which is another way of measuring infected cells rather than the virus – you can always find HIV DNA in people on treatment, so the virus is always there at extremely low levels, largely sitting inside a cell and we can measure it with HIV DNA.
The question we need to answer to find a cure then is where is this low-level DNA and RNA coming from, and how could we eliminate those last bits of persistent virus? We now have a very good idea about where the virus is and where itʼs hiding, which it does primarily in three ways.
The hidden virus
The first is in what we call latently infected T-cells. In a person whoʼs on treatment, we find occasional cells which are infected but that infection is hidden.
Latency is a common strategy that many viruses use to evade the immune system and persist indefinitely in a host – and HIV is a master at it. What HIV does is integrate into the host genome and become silent.
The virus is still there within the cell, but itʼs able to silence itself. And even more brilliantly, it gets into a key infection-fighting cell, whatʼs called a central memory T-cell that’s designed specifically to exist indefinitely because thatʼs our immunological memory.
There are cells that recognise foreign pathogens or new viruses and weʼre armed with a library of different central memory T-cells that persist for life.
We know HIV can always come out of latently infected cells, be activated and released into circulation, if the cell itself is stimulated (although not in a person on ART).
We also know these cells can undergo low-level replication or whatʼs called homeostatic proliferation, so itʼs armed to persist there for life.
The other way the virus can persist is by low-level viral replication. ART blocks most of the replication, but maybe not all of it.
Finally, we know the virus can be sequestered in anatomical reservoirs, the brain being extremely expert at harbouring long-lived infected cells, as is the gastrointestinal tract, urinary tract and lymphoid tissue.
Two models of cure
To cure HIV, we would need to eliminate all HIV-infected cells. This is commonly referred to as a sterilising cure and we now know is really going to be very, very difficult.
The other, perhaps more achievable goal will be to put HIV into remission, or to think of it as we do of cancer. This would mean someone could have long-term health in the absence of ART and the virus would be present but at low levels, less than 50 copies per million. This is now commonly known as the functional cure.
What weʼve learnt over the last few years is that both a sterilising and functional cure are indeed possible, and may be something we could eventually achieve. I will give to one example of each here.
The first to be reported was a Berlin patient named Timothy Brown. He was an American man living in Berlin who needed a bone marrow transplant for leukaemia treatment. He received the transplant from a donor who is naturally resistant to HIV. HIV needs one particular protein to enter a cell, itʼs called CCR5, and about 1% of people do not express CCR5.
Shortly after the transplant, Brown stopped anti-HIV drugs and the virus has not been found in his blood since that time (2009). He is the only example of a sterilising HIV cure, to date that hasnʼt been repeated.
The case caused tremendous excitement because it was an illustration that perhaps cure is possible. Of course, cure could never be done through bone marrow transplantation – highly toxic intervention with a death rate of about 25%. Brown had to have it for his leukaemia but it also cured his HIV.
Then, there’s a group from France called the Visconti patients – 14 people who received very early treatment, which was stopped after three years. The virus remained detectable at very low levels but that’s 14 example examples of a functional cure.
Reason for hope
What these cases have done is given people hope that a cure is possible, and they’ve each influenced many of the ideas and science now being tested to see if we can mimic these cases in other ways.
We could eliminate latently-infected cells by treatment during acute infection or treatment very early or we could activate infection. We could boost HIV-specific immunity, which is important for keeping HIV under control; or by giving a bone marrow transplantation.
Treating acute infection by very early ART (we usually wait until there are signs of immune damage before treatment) could limit the number latently infected cells. It could perhaps prevent this phenomenon of chronic immune activation that fuels ongoing viral replication. It will preserve HIV-specific immunity and it might achieve a functional cure.
But functional cures are still rare, even with very early treatment, and probably only occurs in about 5% to 15% of people. We need to understand better why those 5% to 15% were able to keep their virus under control with the help of early ART.
Other approaches
The other approach is one I have worked on for quite some time, this idea is to actually wake up latent HIV. The principle here is a little bit counter-intuitive.
Latency means that HIV DNA is buried as part the host DNA, sitting inside a resting cell. If we could activate that virus, it would start making copies of itself, and start to make proteins, it would become visible to the immune system.
Usually when the virus leaves the cell, the cell self-destructs. We could potentially wake up the virus and push it out. This would be done in people on antiretroviral therapy, so that if we made any new virus in the presence of treatment, it couldn’t go on to infect new cells.
We now know there are many, many compounds that can do this and we’ve developed many models so we can test and screen different drugs to see which ones can effectively wake up latency in HIV.
One issue with this approach with activating latent HIV is that none of the tools we’ve got at the moment are specific for HIV. Given latent-infected cells are rare – only about one in a million – and we’ve been giving medications that are going to have very significant effects on uninfected cells, it’s a real challenge at the moment.
We have no HIV-specific drugs to wake up the virus. Many people are doing pretty well on one tablet a day, so we need to balance the enthusiasm around finding agents to activate HIV and what could be potentially significant safety issues.
Other strategies worth pursuing include activating and then killing the recently woken cell with something like a therapeutic vaccine. Or making cells resistant to HIV. This latter largely comes through gene therapy, or the capacity to eliminate a gene of interest using – literally – gene scissors.
Proceeding with caution
There have certainly been a lot of advances, interest and development in how we might cure HIV, but there are many more challenges to face. A big challenge is balancing whatʼs acceptable risks and toxicities in a population already doing very well with treatment.
These are not people with malignancy or leukaemia or facing life-threatening illnesses so we really need to think carefully about acceptable risks and toxicities. And also about regulatory and ethical issues.
Thereʼs a big challenge in managing expectations of both the study participants and the community. The cases I’ve mentioned and many others have given many people hope, but we donʼt want to replace that with hype.
Curing HIV really remains a very significant scientific challenge, and weʼre really at only the very first stages of addressing that.
Sharon Lewin receives funding from the NHMRC. She is a member of the International AIDS Society and co-chair of the AIDS2014 conference.